Dieser Beitrag ist auch verfügbar auf:
Deutsch
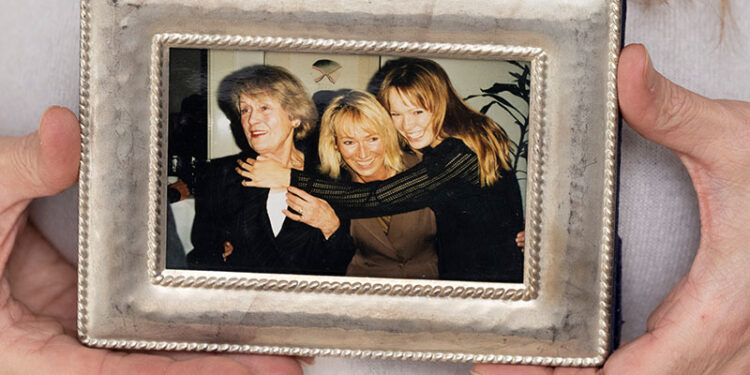
Sophie Rosentreter’s path to becoming a care and dementia expert was not straightforward: She was a model and MTV presenter, lived a life on stage, at high speed. And then there was her beloved grandmother, who suddenly started behaving strangely. In 2000, the dementia diagnosis hit a family that was barely aware of the services available: “Until my grandmother died, I didn’t know that there was such a thing as an Alzheimer’s society.”
It is a sobering realization: If support exists in the early 2000s, it does not reach those who need it so urgently. Powerlessness becomes curiosity, curiosity becomes a calling. Today she knows: Education, knowledge and community bring lightness to care.
In a very personal interview, we delve into the world of Sophie Rosentreter and her grandmother Ilse – and how she develops and communicates solutions for dealing with dementia in care today.
How a family story became a vocation
There are currently officially 1.8 million people with dementia in Germany, over 70 percent of whom are cared for at home. “Family caregivers are the largest outpatient care service, and only a third of them accept help. That is vanishingly small,” says Rosentreter. In contrast to the time when Rosentreter’s family provided care, help and support is available online and offline – and today she is part of the solution.
In 2010, she launched the company “Ilse’s Wide World” and produced films for people with dementia that connect to their emotional world – to memories, gestures and music. She says today about the idea: “I saw in my grandmother’s care facility that the TV program and people with dementia don’t work together. On the one hand, a very fast, cognitive world – and on the other, a very slow, emotional world. Advertising and news also trigger things in people with dementia. We didn’t want that.”
It doesn’t stop at film productions, because she saw: “Before relatives and professional caregivers understand that they can use a movie as a bridge to get back into conversation, a lot of education is still needed.” She delved deeper into communication and activation methods for dementia, such as validation, occupational therapy, basal stimulation and music therapy. Rosentreter: “And suddenly this dark world became very colorful and full of possibilities.” She realized that there are many ways “to shape relationships, to awaken memories and to strengthen the self-esteem of people with dementia.”
Soon she was writing a book, giving training courses in nursing homes, speaking in large halls and making educational films with partners such as the AOK and others.
“Seeking help is a sign of strength”
Sophie Rosentreter still has a lot planned – because there is another personal concern: That family caregivers don’t become a nursing case themselves and burn out. Shortly after her grandmother’s death, her mother also passed away: “I’m sure that she died from the excessive demands and emotional strain of caring for my grandmother.” She herself developed skin cancer and had to have her lymph nodes removed. “Mental pain definitely makes you ill,” she says with certainty. That’s why she talks about it today and helps others to get the support they need.
What would she do differently in a care situation today? “Education, knowledge, support, community – that brings lightness. Having an imaginary suitcase full of knowledge and support at your side brings lightness, and that’s also how we manage to find some beautiful moments in this difficult topic.” She sees our society as “too much in their head”, always wanting to be higher, faster and further. A person who falls ill, whose spirit and mind are declining, has a hard time in this society. But: “The heart does not become demented,” says Rosentreter, and that is exactly what remains when everything else threatens to fade: The feeling, the soul.
What tools and concepts are available for support
Today, there are already a lot of tools and concepts that make life easier. In addition to smart solutions such as intelligent skirting boards and apps, simple adaptations for the home also provide support. An overview is provided by show apartments that can be viewed online and offline.
This is because, for example, color perception and therefore orientation changes with dementia. A white plate on a white tablecloth and a transparent glass of water are simply not visible to people with dementia. A colored plate on a white tablecloth makes food visible; a shot of juice makes the drink “appear” in the glass. The cupboards need clear instructions: Ideally pictograms that provide orientation even when the terms are no longer understood.
Shadows and thresholds are frightening: Doors can be unobtrusively concealed and de-dramatized with curtains. Good lighting close to the floor, for example with socket lights, is important. Non-slip, fixed carpets ensure safety, and a bell or pressure mat alerts you when you get up at night.
In addition to these tips for at home, there are many leisure and relief offers: “Here in Hamburg, there is a dog visiting service for people with dementia in their homes. I get a dog at home and can even take it for a walk. And my relatives can go shopping or just have a cup of tea – or do nothing.” There are already dance afternoons, museum and art programs, even inclusive discos for people who suffer dementia: “There is so much on the market, you have to look around and try out the modules to see: What suits me?”
Care: “There is so much, but on the other hand there is also so little”
In view of the wide range of options, you might think that there is no care crisis – but there is: “A friend is currently looking for a place in a home for her father in Hamburg. She was placed 620th on the waiting list and there are no short-term care places within a radius of 100 kilometers. And that’s just the beginning. We’ve been talking about it for 10 or 20 years, but the masses – the baby boomers – are still to come. And we as a society have to get back into a community, we have to get involved ourselves. The concepts of neighborhood help and neighborhood development exist, but we also have to look at them and help support them.”
Because one thing is clear: The care sector is under pressure and cannot cope with the increasing demand in any way. Care is increasingly being provided at home by family carers, which is increasing their financial and organizational burden. At the same time, the expansion of the highly fragmented outpatient care system is lagging behind market demand and (in Germany and Austria) has developed very differently depending on the federal state. There is no well-thought-out system, only small, regional solutions. “The care insurance funds are on the verge of insolvency, care at home needs to be made more attractive. The system doesn’t work as it is, there needs to be a major overhaul,” says Rosentreter, because: “Poverty through care is also a reality in our country.”
The issue of poverty is multifaceted: It is often not possible to return to work after care, resulting in social isolation and ending up as tomorrow’s care case. “The discussion is always just about the professionals who are now making themselves visible. I think that’s great, but that’s only a small part of it. Care at home must also be recognized and appreciated,” explains Rosentreter.
We would like to thank you for the interview – and this sentence, which summarizes many things and yet never fully explains them, echoes for a long time: “The heart does not become demented.”
Find out more about the products in “Ilse’s wide world” at https://ilsesweitewelt.de
The films are available on DVD and as a stream in the media library.
Find out more about Sophie Rosentreter and your booking as a speaker here: https://www.sophierosentreter.de
Author: Anja Herberth
Chefredakteurin