Dieser Beitrag ist auch verfügbar auf:
Deutsch
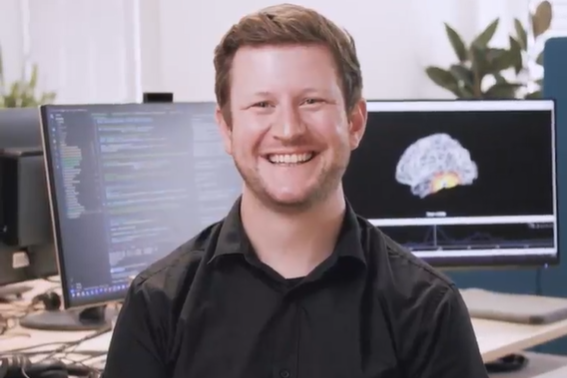
Neurological diseases are on the rise – including diseases such as Parkinson’s, dementia, stroke and depression. Artificial intelligence offers new approaches to treating these diseases and living with them. An interview with Dr. Patrick Reisinger, Data Scientist at the German medical technology company Precisis, about new treatment options using artificial intelligence and a healthcare system that is increasingly reaching its limits.
Neurological diseases affect our nervous system – including diseases such as epilepsy, stroke, multiple sclerosis, migraine, Parkinson’s disease and dementia. Depression also often has neurobiological causes. These are diseases that have developed massively in recent decades: The number of cases worldwide has risen by 59 percent since 1990, and more than 3.4 billion people are affected. The number of Alzheimer’s and Parkinson’s diseases could double by 2050.
Drug therapies are usually the first treatment option. However, this classic approach is not enough – because what happens if the medication does not work and the side effects are a major problem? What if brain surgery poses too high a risk? For this reason, alternative treatment methods are being researched. One of these approaches is neurostimulation, which has been in use for epilepsy since 2022.
How neurostimulation works
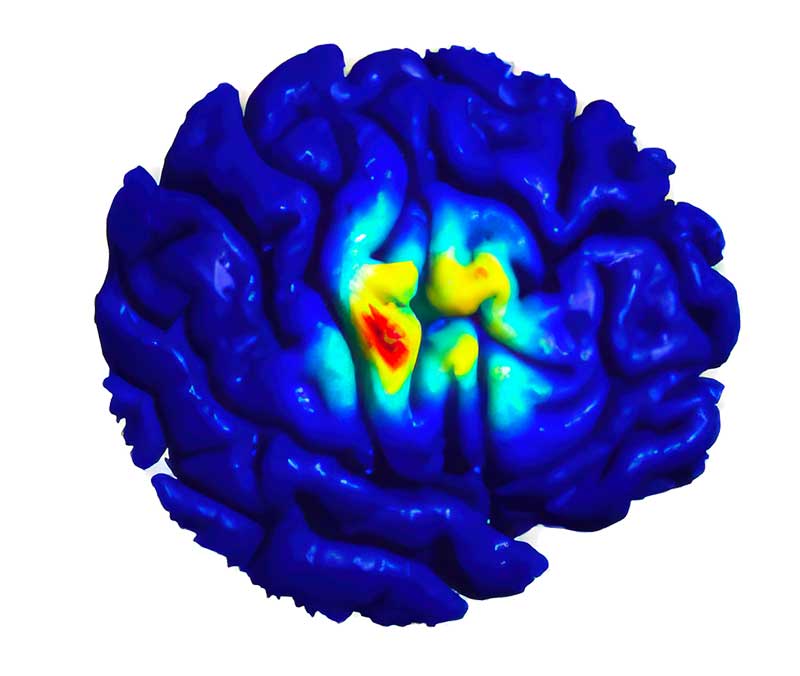
Neurostimulation acts like an intelligent clock for the brain – it balances out over- and underactivity in a targeted manner. Put simply, when neurons in the brain fire excessively and overload it, it is stabilized. If there is too little brain activity, as in the case of depression, it is stimulated. Neurostimulation for epilepsy works in two different ways. The first emits small, rapid pulses at short intervals during the day to prevent seizures at an early stage. The second type of stimulation usually runs once a day, often in the morning, and sends slow pulses over 20 minutes to calm the brain and stabilize it in the long term.
In the future, artificial intelligence will be used to monitor the brain in real time, predict seizures and react to them immediately.
Another option is to suppress seizures that are building up: “Our patients have a small remote control with which they can initiate neurostimulation themselves if they feel an epileptic seizure building up.”
The good news is that these new procedures do not require the skull to be opened. “The electrode is simply implanted under the scalp and is connected to a stimulator in the chest via an invisible cable. The stimulation takes place through the skull bone. This is a much more direct and personalized approach than with medication,” explains Dr. Reisinger.
Overall, neurostimulation still plays a subordinate role, but is becoming increasingly important in selected cases – for example in cases of drug resistance or when surgery is simply not possible. This is the case, for example, when sensitive areas of the brain are affected and patients would be blind after an operation.
AI: more precise, personalized medicine in real time
Artificial intelligence is paving the way for these new procedures, which will enable personalized therapies and treatments in the future. “AI is excellent at recognizing patterns and anomalies. The idea is that AI could control the electrodes in the implant even more specifically, based on individual patterns and brain activity,” explains Dr. Reisinger. This form of therapy could learn independently when the implant should best stimulate. “AI could also help us to understand the brain before a seizure occurs,” says Reisinger. This could not only increase the speed of diagnosis, but above all the precision and effectiveness of therapy.
How long will it take for this form of therapy to be approved with the help of AI? “We are less than 10 years away from market approval, which is a very short period of time in the development of new forms of therapy. We want to start clinical trials in the next few years. This will happen very quickly,” says Dr. Reisinger.
What it would need above all: Data. Because an AI can only learn if data is available for training. Reisinger: “It would be enough if more was made available for scientific research. Internationally, the same Children’s Hospital Boston-MIT data sets with 22 patients are often used. Of course, I know that data protection is a difficult issue, but data is simply essential for the development of new, reliable therapeutic approaches.”
Innovation from Europe: The AI Act as a challenge
Innovations in neurostimulation today go far beyond pure technology. They require data, precision – and a responsible approach to regulation. The European AI Act in particular is the subject of intense debate in the industry. “Of course, the AI Act poses challenges,” says Dr. Patrick Reisinger. “But we also see it as an opportunity: anyone who sets standards here shows that safe, effective AI-based medicine is possible.” In this case, pioneering work also means developing future-proof intelligent implants in compliance with the legal framework.
The FDA, the US Food and Drug Administration, has already classified EASEE, the neurostimulation for epilepsy, as a “Breakthrough Device Designation”: This is a program to accelerate the development and testing of drugs for serious or life-threatening diseases. The aim is to make promising therapies available to patients more quickly. We can only hope that Europe will learn from this.
More about Precisis at: www.precisis.com
Author: Anja Herberth
Chefredakteurin